HELENA — Earlier this year, Montana regulators began determining whether people can remain on the state Medicaid program – for the first time since the end of the national COVID public health emergency. Now, they’ve released the first data showing how many Montanans have had their coverage expire so far.
During the COVID emergency, the federal government directed that everyone on a state Medicaid program could remain enrolled without having their eligibility reconfirmed. That requirement ended on April 1, so regulators must recheck most recipients’ eligibility annually and when they report changes like getting married or divorced or having a child.
Leaders say there are a number of reasons why someone might no longer be eligible for Medicaid, but one of the most common is that their income rises out of the qualifying range.
In March, Montana had 324,125 residents enrolled in the Medicaid and Healthy Montana Kids programs. The Montana Department of Public Health & Human Services plans to go through the redetermination process with all of them over a ten-month period.
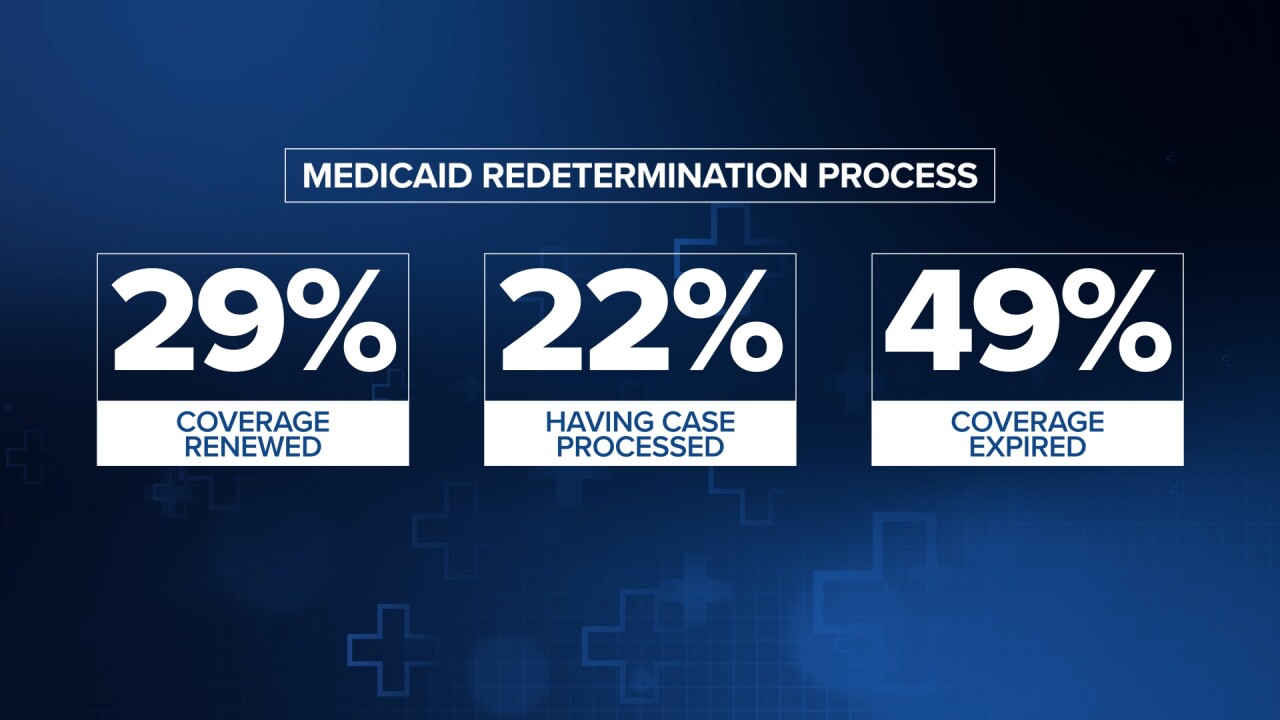
During the first month, April, DPHHS worked with 31,596 individuals. As of June 15, about 29% of those had their coverage renewed, 22% submitted additional information and the department is still reviewing their cases, and 49% had their coverage expire.
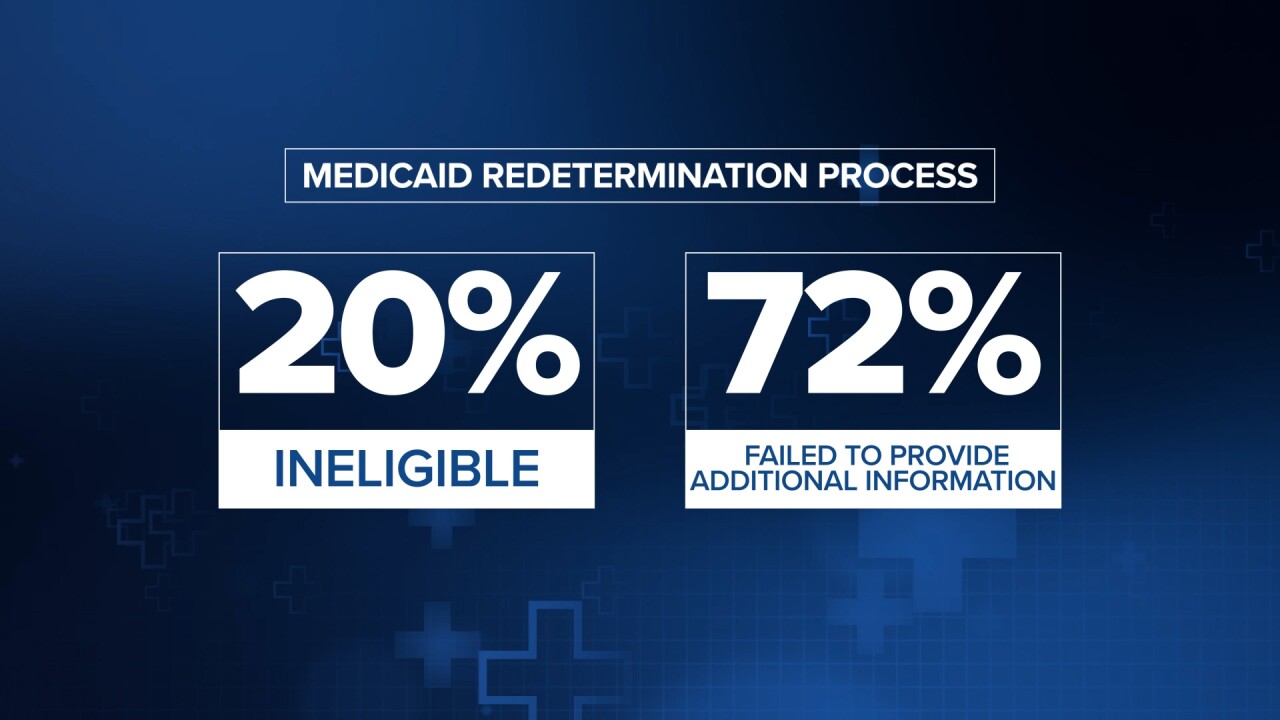
Of the 15,471 individuals who lost coverage, DPHHS says 20% of them were determined to be ineligible, while 72% failed to provide the additional information the department asked them for.
A spokesperson for DPHHS says the department is prioritizing people who they thought were more likely to no longer be eligible, so they expect a higher percentage of people will be removed from the program in the first few months. They said that could also explain why so many people didn’t return the information DPHHS asked them for.
“When people are aware that they no longer meet eligibility criteria, they would not necessarily make the effort to complete and return paperwork,” they said.
The department says people who didn’t return the requested information received multiple follow-up messages and reminders.
When the redetermination process began, leaders urged Medicaid recipients to provide updated contact information so they would be sure to get the paperwork DPHHS was sending them. DPHHS says they’ve sent about 100,000 text messages to households to remind them to update their information, and only 3% of the closed cases were because the mailings were returned without a new address.
The spokesperson said the department has focused on people who qualify based on income so far, with those qualifying based on age or disability set to begin in July.
The data for May is still being processed. DPHHS reports 40,334 individuals went through the redetermination process that month. So far, almost 21% have had their coverage renewed, 35% have provided additional information and the remaining 44% have not yet returned the requested information.
DPHHS has teamed up with Cover Montana to help those who do lose Medicaid coverage prepare for the next steps. Cover Montana is a network of organizations, including the Montana Primary Care Association, that helps people understand and get connected to health insurance options. You can find local help in your area by going to covermt.org, or call Cover Montana’s Help Line at 1 (844) 682-6837.
The department also says those who have lost coverage can reapply at any time by going to apply.mt.gov, visiting a DPHHS Office of Public Assistance or calling the Public Assistance Helpline at 888-706-1535.
TRENDING



